It is now ten years ago that the first students started their journey in the Surgical Training Programme (STP) in Sierra Leone. This was the start of CapaCare providing training in life-saving surgical and obstetric skills. The vision of the organisation is to contribute to sustainable healthcare systems through capacity building in underserved populations. During 2021 we want to reflect on the last ten years by interviewing two people every month that have played an important role in the development of the organisation and Programme. This month we start with the two founding members of the Programme, Håkon Bolkan and Brynjulf Ystgaard.


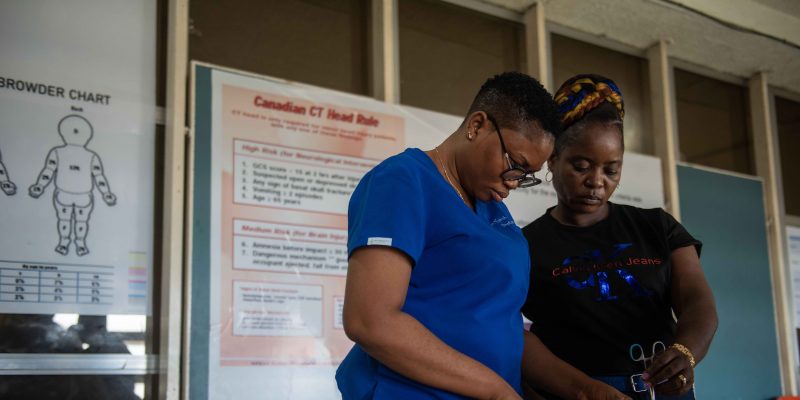
Trauma course at Masanga
- Can you describe briefly what your role is or has been in CapaCare?
Together with Brynjulf, Håkon founded CapaCare and has been chairing the organisation in different ways since. Both had been working on relief missions abroad, with MSF and the Red Cross Movement respectively. These missions had more or less been of the “there and back again” type. Both Brynjulf and Håkon felt the need for a venture with a lasting impact on the recipient society. The opportunity presented itself when Håkon and his wife, Ellen were heading to Sierra Leone to work for MSF in Bo. “Brynjulf asked if we should engage in surgical training in Sierra Leone, maybe start a project where we could teach local doctors to operate hernias.” Some months into the stay in Sierra Leone, they got a visitor at the MSF hospital, a Danish surgeon who was renovating a hospital in a very remote and small place called Masanga.
This surgeon, Peter Bo Jørgensen, invited Håkon to visit Masanga hospital. A long weekend in February 2008, together with Dr Frank Vraaji from the Netherlands, convinced him that this could be a suitable location for a surgical training programme.
Back in Norway, discussions started on how, what, when and with whom. Six years after the horrible civil war in Sierra Leone, there were few doctors in the districts. With MSF, Håkon had worked with Community Health Officers (CHOs), and found this group to be eager, hard-working, ambitious and both willing and very suitable candidates to train. Although their training and name indicate preferences for community medicine, many CHOs were working inside hospitals. Some of those again were ad-hoc trained and performed surgery.
A challenging part in the early days was funding. Surgical training is not something to do for a few years. The challenge was that long term financial commitments were not possible to establish based on good ideas only, and that offering training to people without financial security was irresponsible. Luckily, they had contacts within the Lions club, initially through Ellen’s uncle Karstein. After several meetings with and presentations to the Lions club in central Norway, Lions adopted the surgical training programme as their international priority project. This gave Brynjulf and Håkon some reassurances that some funding was secured.
However, the support from Lions was not sufficient, they needed additional investment to get started. Around the same time, Ellen and Håkon decided to get married and they saw this as an opportunity to launch a fundraising event. After many years together their need of hardware of any kind was not too pressing. Instead of kitchen tools and other popular wedding gifts, they encouraged their guests to make a donation to the plans for surgical training in Sierra Leone.

The drawing in the middle symbolises the donation from the wedding guests and was handed over to the hospital director Thomas Fortune in 2009. The drawing can still be found in the CapaCare office
- How has CapaCare impacted your life?
Ellen and Håkon being newlywed, what could be more romantic than inviting his boss to join them in Sierra Leone for the honeymoon? Together with Brynjulf and his wife Lise, they visited Masanga hospital, potential partner hospitals and Ministry officials. They sounded out potential stakeholder’s interest in collaborating on a surgical training programme. Through long talks and discussions, the programme started to take shape. Not everyone they met in Sierra Leone was overly enthusiastic, to put it mildly. However, some were, one of them being Dr Donald Alpha Bash-Taqi, Sierra Leone’s only paediatrician. As Director of Training within the Ministry of Health and Sanitation (MoHS), he had attended a workshop in Ethiopia about task-sharing in surgery and obstetrics a few years earlier. Dr Bash-Taqi became an invaluable ally and promotor of the task-sharing programme. Clearly, the small seed planted two years earlier started to mature. Håkon says, “Ellen and I made jokes, that this undertaking would be our first child, and it would likely be a long time parenting it.”

Honeymoon picture – grand tour at the Masanga Hospital
3.Can you tell one personal CapaCare story that you never will forget?
After the honeymoon-trip, there were several others, always involving visits to the Ministry of Health in Freetown to lobby, both for the programme and for the cause to push surgical care and training on the governmental agenda. Brynjulf and Håkon considered collaboration with and involvement of the government as crucial to develop a sustainable surgical programme. After many meetings without tangible progress, they decided the best they could hope for in terms of governmental approval was permission to do a small pilot, to validate the concept. The strategy was to train in total two or three young doctors or Community Health Officers in surgery and obstetrics, each for three years. They would then undertake an evaluation, and if successful, later negotiate a scale-up.
During a visit to Sierra Leone together with Peter, they were able to secure an audience with the Minister of Health, Zainab Hawa Bangura, who at that time also served as the Minister of Foreign Affairs and International Cooperation. As a female politician promoting human and women’s rights in Sierra Leone she was well acquainted with the poor statistics for maternal health in her country. Very high, if not on the top of her agenda was the extreme maternal death ratios. Sierra Leone was at that time considered the most dangerous country in the world to deliver a baby. Less than 1% of women living in rural areas delivered their child through a caesarean section, and that the lack of skilled personnel to do this crucial lifesaving procedure within her district governmental hospitals contributed to the devastating maternal statistics. Håkon says, “Knowing we had to grasp her attention with a few sentences, we boldly stated that we could help her doubling the number of caesarean sections in governmental hospitals within a few years and that this would have a massive positive impact on emergency obstetric care for women living in rural areas.”
Midway into the presentation she interrupted and directed them to wait. She asked her secretary to summon available Directors in the Ministry of Health for an immediate meeting. In front of around 20 of these dignitaries, Håkon and Peter were asked to start over and got the chance to elaborate further and in more detail regarding their intentions. Towards the end of the presentation the Minister asked how many they could train. Without having had the chance to discuss this, Peter and Håkon looked at each other knowing that this was their chance. In front of the Minister and her Directors, Håkon made some very quick calculations and said with conviction, “why not aim for two-three at each district hospital, 12 hospitals in total outside the capital. We can train 30 in five years.”
They got the necessary approval to start the programme and later signed a Memorandum of Understanding with the Ministry of Health and Sanitation, as an addendum to the contract Masanga Hospital had with the government. On the way out of Freetown after the meeting they were all thrilled by this sudden development. Håkon says, “in the late afternoon rush-hour traffic jam, Peter in the front seat could not hold back anymore. He opened the window and recited parts Dr Martin Luther King Jr’s I-Have-a-Dream-speech.”
On a more sombre note, they also recall a number of patients encountered on their sojourns to Sierra Leone. One was a lad of 20, admitted to Masanga with respiratory distress. He died of poliomyelitis affecting the intercostal muscles and the diaphragm, with no possible treatment available. A jab of vaccine would have saved this poor chap’s life. Another was a woman in her 30s, presenting with an ulcerating mammary tumor. For her they could do surgery, if nothing else. They saw har again after two years. What happened afterwards, they do not know. And histopathology? At that time, they had to send the specimen to Ghana, and that simply was not on.
 Meeting in the Ministry of Health And Sanitation (MOHS); 1st from right: Founder of the Masanga Rehabilitation project Dr. Peter Bo Jørgensen, 3rd from right: Current Chairman of Masanga International Dr Eddie Cole, 4th from right: Director of Training and Research MOHS Dr Donald Alpha Bash-Taqi, 5th from right: Chief Medical Officer in Sierra Leone Dr. Dao, 6th from right: Danish volunteer/Masanga Denmark board Pernille Dixen, 7th from right Håkon A. Bolkan
Meeting in the Ministry of Health And Sanitation (MOHS); 1st from right: Founder of the Masanga Rehabilitation project Dr. Peter Bo Jørgensen, 3rd from right: Current Chairman of Masanga International Dr Eddie Cole, 4th from right: Director of Training and Research MOHS Dr Donald Alpha Bash-Taqi, 5th from right: Chief Medical Officer in Sierra Leone Dr. Dao, 6th from right: Danish volunteer/Masanga Denmark board Pernille Dixen, 7th from right Håkon A. Bolkan
- What is your hope for the future of CapaCare?
In the long run, the hope is that CapaCare will continue to attract enthusiastic, professional, eager and motivated health care workers under the vision that quality healthcare is for all. Brynjulf and Håkon also hope that CapaCare will be true to the organisation’s mission and contribute to sustainable healthcare systems through capacity building. They hope the organisation will keep focusing on the most underserved of societies and that the sharing of medical knowledge and skills remain the core principles of CapaCare’s endeavour.
Brynjulf says, “we hope we will be true to our values in the future, always seeking collaboration with governments and promoting partnerships. We will remain research oriented and continue to apply international standards to our work. Among the populations we support, we hope we will be able to stimulate accountability and foster empowerment.”
In the short run, Brynjulf and Håkon hope CapaCare will be more successful in pushing for adequate recognition, remuneration and regulation of the graduates of the Surgical Training Programme in Sierra Leone.